Paediatric rheumatic diseases
Rheumatic diseases also affect children and adolescents
Rheumatic diseases are generally regarded as diseases of older people, however, children and adolescents can also suffer from such conditions. Chronic inflammatory rheumatic diseases affect at least 20,000 children and adolescents in Germany. The most common form is juvenile idiopathic arthritis (JIA), a chronic inflammation of the joints. JIA is a heterogeneous disease, with the various forms of the disease differing according to the number of joints affected and organ involvement (e.g. skin).
In addition to JIA, the term “Paediatric rheumatic disease” covers a number of other conditions, including connective tissue diseases such as systemic lupus erythematosus (SLE), or dermatomyositis. In this group of diseases, very complex inflammatory processes can take place in almost all body tissues. In the long run, an early diagnosis and proper treatment is crucial in preventing permanent joint or organ damage, and to maintain the quality of life for young people suffering from rheumatic disease.
JIA has many faces
Juvenile idiopathic arthritis (JIA) is the most common inflammatory rheumatic disease in young people: about one in 1,000 children and adolescents is affected, amounting to an estimated15,000 children and adolescents in Germany. JIA manifests itself in many different ways and is therefore often difficult to diagnose. The clinical picture ranges from inflammation of a single joint or a few joints (oligoarthritis), to inflammation of many joints (polyarthritis), to a highly acute febrile illness with skin rash (arthritis with a tendency to enthesitis) and inflammation of internal organs (systemic JIA, psoriatic arthritis). The different manifestations of JIA are grouped into several categories.
Typically, children affected by JIA develop the disease at the age of 2-3 years. At this young age children are not yet able to verbally express their pain, therefore it is typically the parents who notice that their children have swollen joints and/or that they are moving less, differently and/or keeping restrained postures.
JIA versus adult rheumatism
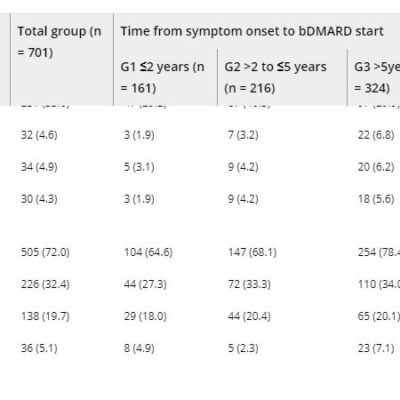
Juvenile idiopathic arthritis differs significantly from adult rheumatic diseases in its clinical manifestation, possible comorbidities and prognosis. However, they do have one thing in common: the treatment has to be consistent and long-term. The earlier the treatment, the better the outcome. A combination of medication, physiotherapy, ergotherapy, orthopaedic therapy and psychosocial measures is usually applied. The therapy goal is no longer just to alleviate the symptoms, but to suppress the rheumatic inflammation entirely so that the children and adolescents affected can lead a normal life with as high a quality as possible.
Optimal care for young people with rheumatic diseases
In order to achieve optimal care for young people with rheumatic diseases, the first step is to evaluate the current care situation. This includes both the rheumatological care and the assessment of the medical, psychosocial and economic consequences of the diseases. Important questions include:
- How quickly after disease onset do affected adolescents see a rheumatologist?
- Which medications are prescribed at the beginning and in the further course of the disease?
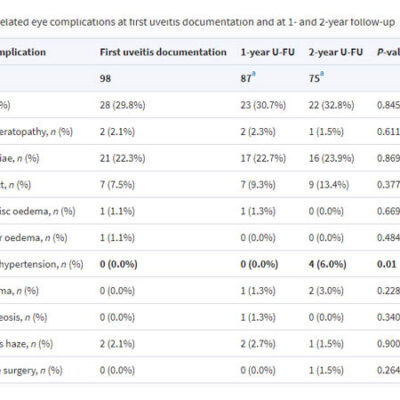
- Which comorbidities can occur during the course of the disease?
- How do affected adolescents deal with their disease?
Large cohort studies specifically address these questions.
Cohort studies: Data collections for improving care of young people with rheumatic diseases
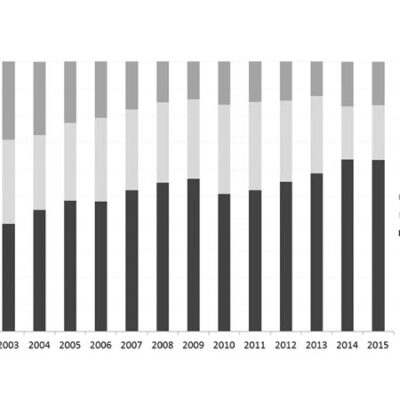
Three large nationwide cohort studies on paediatric rheumatology form the basis of the epidemiological research carried out at the DRFZ,which have been carried out in cooperation with doctors and “Rheumazentren” for many years:
- the national database of children and adolescents with rheumatic disease, which records almost 14,000 patients per year throughout Germany,
- the JIA early cohort ICON with 975 JIA patients and about 500 healthy controls,
- the JuMBO biologics register for young adults with JIA with over 1,700 participants.
More information and results on these cohort studies and other linked projects can be found here: research group Paediatric Rheumatology and Health services research
Understanding disease processes in JIA
Besides the epidemiology, the DRFZ also investigates the mechanisms underlying Juvenile idiopathic arthritis (JIA). JIA is a so-called autoimmune disease as the immune system turns against its own body. Different cells of the immune system initiate an excessive immune response that leads to chronic joint inflammation. It is assumed that certain environmental influences, such as infections and diet in children with certain genetic conditions, also influence the inflammatory process. However, it has not yet been possible to decipher the underlying cause of this misguided immune response.
Using state-of-the-art techniques, researchers can characterise the properties of individual “inflammatory cells” with high resolution (e.g. “single cell sequencing “). Since cells migrate from the blood into the joint and back again, the analysis of blood cells can be used to investigate disease processes in the joint. The detailed analysis of inflammatory processes help the researchers to:
- decipher causes of chronic inflammation,
- describe markers that can be used for diagnosis and therapy monitoring,
- and to identify possible therapeutic approaches.
more information can be found here: Research Group Chronic inflammatory diseases in childhood and adolescence
In a new joint research project of the DRFZ and Charité, corresponding analyses are being carried out in children with JIA who are observed over a longer period of time (Targ-Art ). In this project, another central question being asked is why some young patients experience a spontaneous remission (regression) of the disease, while others do not.

 Deutsch
Deutsch