EBV reactivation as a key mechanism of MIS-C after SARS-CoV-2 infection
Why children become seriously ill weeks after a Covid-19 infection and how they can be cured
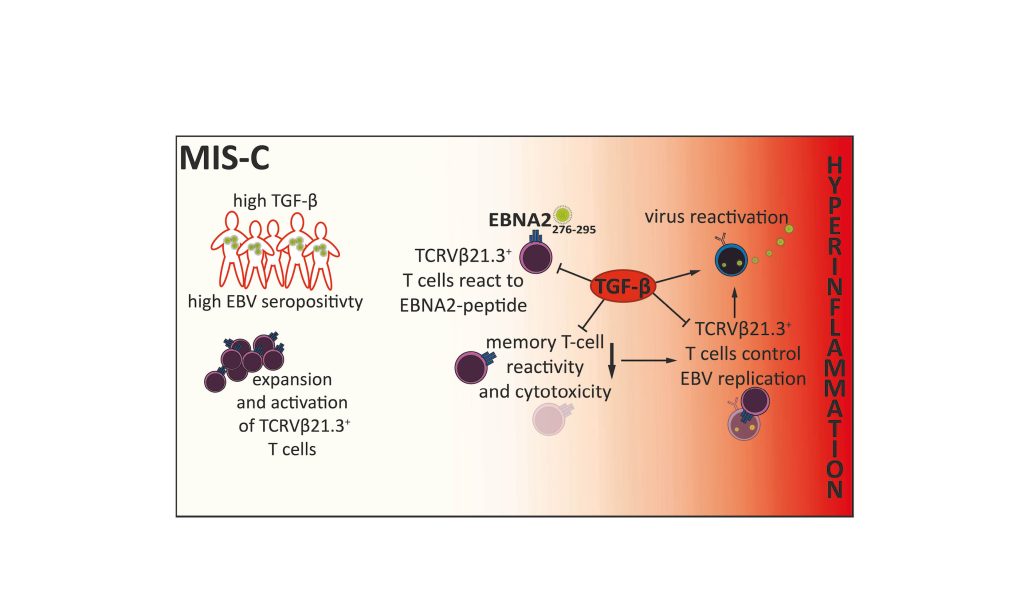
Researchers from Dr. Mir-Farzin Mashreghi’s group from the German Rheumatology Research Center Berlin (DRFZ), a Leibniz Institute, and Prof. Dr. Tilmann Kallinich’s group from Charité – Universitätsmedizin Berlin and Liaison-Group leader at DRFZ, have gained important insights into multisystemic inflammatory syndrome in children (MIS-C). This rare but severe disease occurs 4 to 8 weeks after a SARS-CoV-2 infection and is caused by impaired reactivity of memory T cells. The cytokine TGF-β plays a central role here: it impairs the function of T cells, triggers reactivation of the Epstein-Barr virus (EBV) and amplifies the systemic inflammatory reaction. A targeted blockade of TGF-β was able to effectively interrupt these mechanisms in the study. The results were published in the high-ranking journal Nature.
The joint DRFZ and Charité study shows that acute MIS-C is characterised by a significant restriction of the reactivation of virus-reactive memory T cells. This dysfunction is caused by elevated serum TGF-β levels, as observed in severe COVID-19 cases in adults. “As a result, T cell-mediated surveillance and elimination of latent viruses, especially EBV, is severely impaired”, the first author, Dr. Carl Christoph Goetzke emphasizes.
The researchers found that in MIS-C patients, a specific T cell expansion of EBV-reactive cells occurred, which were unable to eliminate infected cells due to the increased TGF-β levels. At the same time, the high TGF-β levels led to reactivation of EBV in B lymphocytes. This uncontrolled multiplication of the virus contributed decisively to the severe systemic inflammatory reaction. By blocking TGF-β, the functionality of the T cells was restored and EBV reactivation in infected B lymphocytes was prevented.
The impairment of T cell reactivity caused by TGF-β clearly correlates with an increased EBV concentration in activated B lymphocytes from the blood. Children who developed MIS-C after a SARS-CoV-2 infection were more likely to have antibodies against EBV in their blood than control groups of the same age who had also undergone a SARS-CoV-2 infection but did not develop MIS-C. A key finding from this observation is that children with latent EBV have an increased risk of developing MIS-C after a SARS-CoV-2 infection.
The results of the study highlight the complex relationships between SARS-CoV-2 infections and secondary diseases, especially in children. They also provide valuable information for the development of targeted therapies for the treatment of MIS-C and other post-COVID-19 diseases that may be associated with EBV reactivation.